Abstract
Background: A comprehensive evaluation of woman-specific risk factors in relation to incident heart failure (HF) is limited.
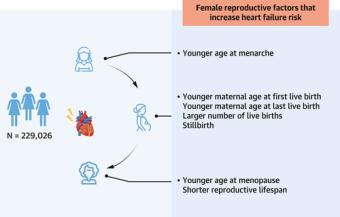
Objectives: The study sought to investigate the association of multiple female reproductive factors with the risk of HF.
Methods: Between 2007 and 2010, 229,026 women (mean age: 56.5 years) without prevalent HF from the UK Biobank cohort were included and followed until December 2020. The relation between (self-reported) reproductive factors and HF was analyzed using Cox proportional hazards models with adjustment for potential confounding.
Results: Menarche at age <12 years, compared to age 12-13 years, carried a 9% larger risk of HF (HR: 1.09 [95% CI: 1.01-1.18]). Younger age at menopause was associated with a higher risk of HF (HRage < 45 y vs 50-51 y: 1.15 [95% CI: 1.03-1.28]; HRage 45-49 y vs 50-51 y: 1.11 [95% CI: 1.01-1.23]). Younger maternal age at first live birth (HRage < 21 y vs 24-26 y: 1.42 [95% CI: 1.28-1.59]; HRage 21-23 y vs 24-26 y: 1.14 [95% CI: 1.03-1.26]) and at last live birth (HRage < 26 y vs 29-31 y: 1.19 [95% CI: 1.07-1.33]) were associated with higher risk of HF. Compared to women with 1 or 2 children, having 3 or 4 children (HR: 1.09 [95% CI: 1.02-1.17]) or >4 children (HR: 1.24 [95% CI: 1.05-1.47]) was associated with higher HF risk. Experiencing miscarriages or abortions was not significantly associated with incident HF, whereas experiencing 1 stillbirth and recurrent stillbirths conferred a 20% and 43% larger risk of HF, respectively, compared to no stillbirth.
Conclusions: The findings emphasize the importance of female reproductive history in the assessment of HF risk.
