August 2020
Contact: Rachel Linn
Email: RLinn@civhc.org
Report Insights:
- Use of telehealth services was rising before the onset of the novel coronavirus pandemic.
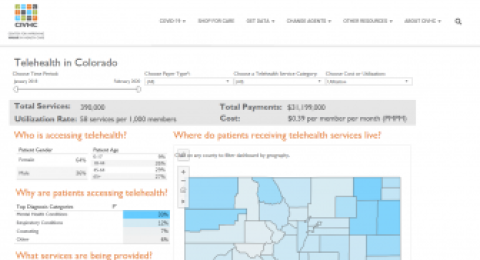
- From January 2018 to February 2020, telehealth utilization visits per 1,000 members increased from 57 to 75.9 (33%) for commercial, 28.9 to 55.1 (91%) for Medicaid and 125.7 to 142 (13%) for Medicare Advantage members.
- Females use telehealth services more often than males (64% compared to 36%), and young adults aged 18-44 use telehealth services more than other age group.
- Across all payers, mental health conditions were the most frequent reason for telehealth visits (33%) followed by respiratory conditions (12%) and counseling (7%), though the top diagnoses varied significantly by payer type.
- Primary care providers have historically provided most telehealth services, followed by behavioral health providers.
- Alamosa county leads the state with the highest overall telehealth utilization rate, with 93% of the visits in that county for mental health conditions.
- From January 2018 to February 2020, commercially insured patients increased their use of telehealth to access behavioral health providers by 83%.
